This informal CPD article ‘Gonococcal infection antibiotic resistance and its wane on the introduction of ceftriaxone and Cefixime’ was provided by Nwaobia Hope Olileanya from The Edge Medical Writing, an organisation that provides high quality medical writing support, tailored to meet the needs of medical education, product development, and the dissemination of medical information.
Most bacterial infections keep emerging and re-emerging as one choice of antibiotic has been used in combating them; Gonorrhea is one of them. Gonorrhea is a sexually transmitted disease caused by infection with the Neisseria gonorrhoeae bacterium. Neisseria gonorrhoeae is a Gram-negative diplococci bacterium.
Pathogenesis
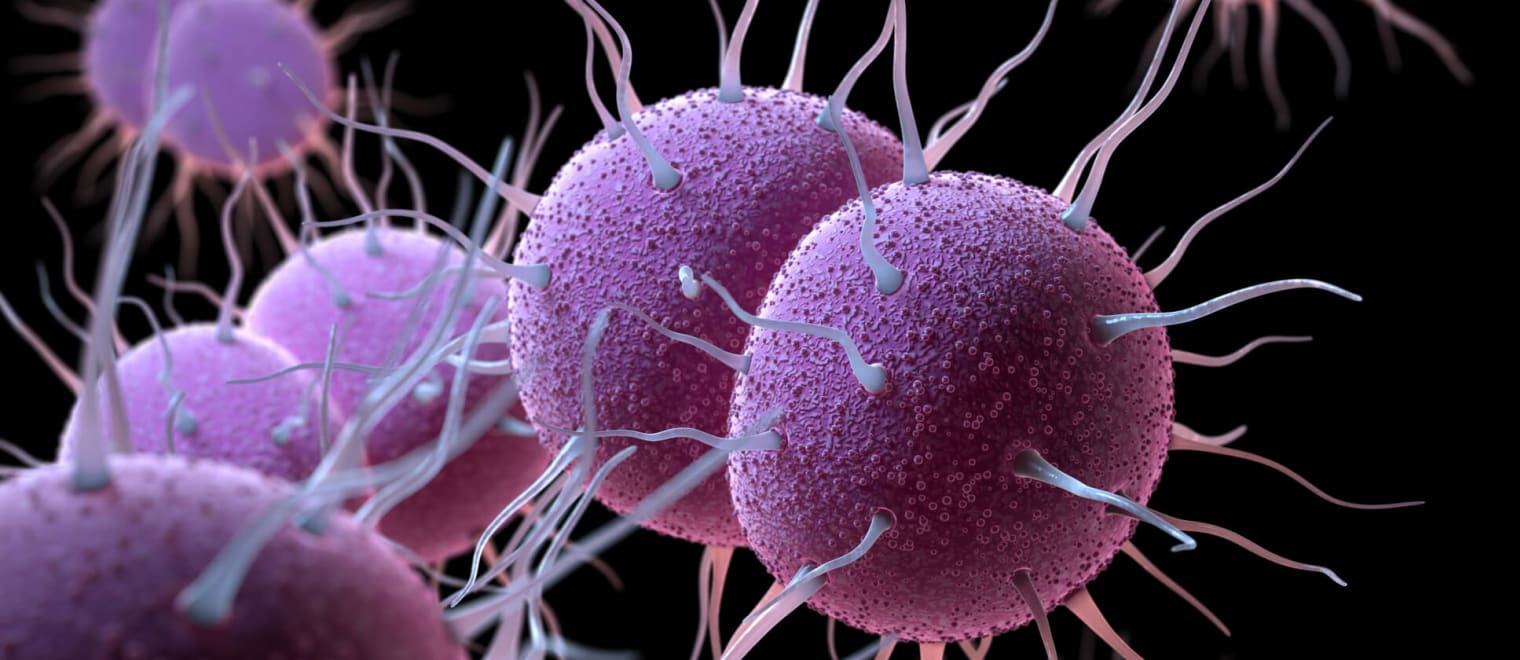
Gonococci selectively attaches to specific non-ciliated epithelial cells of the body, notably those of the urethra, uterine cervix, pharynx, and conjunctiva. Infection begins when the fimbriae from their surface attach specifically to receptors on host cells(1). These pilli(fimbriae), and other surface proteins such as Opa protein, possessed by Gonococcus express different surface antigens which allow them to attach different kinds of cell receptors and also will enable them to escape the effects of antibodies formed against them(2).
Like other pathogens, Gonococcus produces an enzyme that destroys IgA antibodies found on mucosal surfaces. Opa proteins of the outer membrane of Gonococcus represent another important pathogenicity(1). These proteins attach specifically to receptors on CD4 T lymphocytes, thereby preventing activation and proliferation of the lymphocytes and impairing the immune response to the infection(3).
Gonococcus epidemiology in Africa
The World Health Organization (W.H.O) estimates that in 2020, 82.4 million new cases were infected among adolescents and adults aged 15-49 years world-wide, with a global incident rate of 19 per 1000 women and 23 per 1000 men(1). Sequel to the estimate, The W.H.O noted that 7.5 million people in Africa had Gonorrhea(6). The prevalence was higher among females, with about 4.3 million people infected, whereas the number of males affected was 3.2 million(1). The WHO has estimated that every year in Africa there are 16 million cases of Gonorrhea-about 1.5 million case per year in Nigeria (College of Medicine, University of Ibadan)(7).
Diseases associated with gonococcus infection
Sexually transmitted diseases in pregnant women can result in pre-maturity, stillbirth and neonatal infections which Gonorrhea is among them. Gonorrhea follows a different course in women(1). Besides infecting the urethra, gonococci thrive in the cervix and fallopian tubes, as well as in glands in the vaginal wall and other areas of the genital tract(1). 15% to 30% of untreated infections progress upward through the uterus into the fallopian tubes, causing pelvic inflammatory disease (PID)(1). In some cases, the infection exists in the fallopian tube and passes into the abdominal cavity, which attacks the surface of the liver or other abdominal organs(9).
Though the movement of gonococcus to the uterus is not well understood there is a possibility that the organism attaches to the sperm(2). When the fallopian tube is scarred, the passage of the ova is blocked, which causes sterility and dangerous complications in which the embryo develops in the fallopian tube or even in the abdominal cavity outside the uterus (ectopic pregnancy)(9). Gonorrhea in most women can be asymptomatic as the organism attaches to the wall of the birth canal(10). During the time of labor, the baby picks the gonococcus from the birth canal, which leads to Ophthalmia neonatorum: blindness in new born babies(10).
In men, Urethritis leads to a burning sensation during urination and the production of purulent discharge from the urethra(10). The discharge may be foul smelling, if untreated can result to scarring of the urethra. It can transmit to the testes, causing orchitis and high chances of prostate cancer(10).